Voice care
See also free voice care literature and UK Voice Clinics directory
Reflux and your Voice
by Sara Harris, Speech and Language Therapist specialised in Voice Disorders and Sara Caldwell, Speech and Language Therapist specialised in Voice Disorders. With grateful thanks to Cathinka Guldberg, Speech and Language Therapist specialised in Swallowing Disorders, Tom Harris, ENT Surgeon/Laryngologist and John Rubin, ENT Surgeon / Laryngologist.
What is acid reflux?
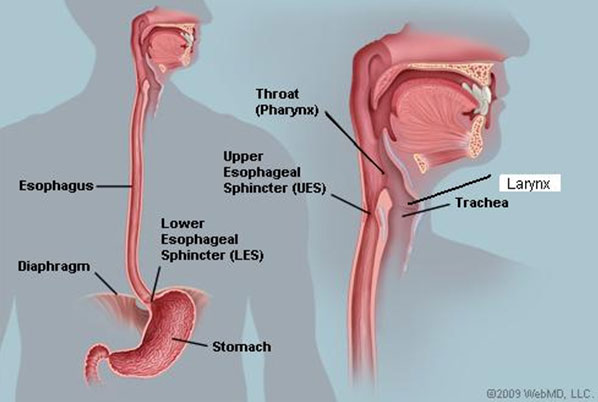
Stomach juices are made up of strong digestive acids, containing enzymes to break down our food and bile from the gall bladder to emulsify fats. The stomach lining is designed to cope with these juices but sometimes they travel upwards from the stomach into the gullet (oesophagus) which was not designed to accommodate powerful digestive juices and the oesphageal lining becomes irritated causing symptoms of indigestion (heartburn). This process is referred to as gastro-oesophageal reflux (GOR).
However, in some people, small amounts of stomach juice can spill back into the upper throat (pharynx) affecting the back of the voice box (larynx) causing irritation and hoarseness. This is known as laryngo-pharyngeal reflux (LPR). It is often called 'silent reflux' because many people do not experience any of the classic symptoms of heartburn or indigestion.
LPR can occur during the day or night, even if a person hasn't eaten anything. Usually, however, LPR occurs at night.
The term reflux comes from a Greek word meaning 'backflow'. Normally, the things we eat and drink stay in the stomach to be digested and do not spill back up into the oesophagus. However, if the valve at the lower end of the oesophagus (the oesophageal sphincter) is weak or disco-ordinate reflux may occur.
What are the symptoms of LPR?
The most common symptoms of LPR are:
- A sensation of food sticking or a feeling of a lump in the throat
- A hoarse, tight or 'croaky' voice
- Frequent throat clearing
- Difficulty swallowing (especially tablets or solid foods)
- A sore, dry and sensitive throat
- Occasional unpleasant "acid" or "bilious" taste at the back of the mouth
- A feeling that too much mucus/phlegm is collecting in the throat
- Sudden coughing or choking spasms at night
- Chronic cough
- Excessive burping, particularly during the day
Heartburn
Some people with LPR also experience heartburn. Others rarely notice heartburn or never experience it at all (hence the term 'silent reflux'). This is because the material that refluxes (refluxate) does not stay in the oesophagus for long. As a result, the contents do not have enough time to irritate the oesophagus and cause heartburn.
However, if even small amounts of reflux come all the way up into the pharynx and larynx, other problems can occur. This is because the tissue lining the larynx and pharynx is more sensitive to injury and irritation from stomach juices than the lining of the oesophagus. Damage to the larynx from stomach refluxate will affect a person's voice and can sometimes affect their lungs and breathing.
A lump in the throat

A healthy larynx
Image courtesy Tom Harris
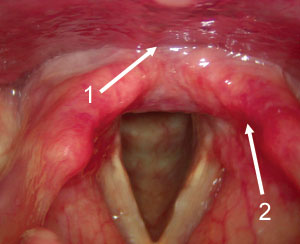
A larynx showing signs of reflux
Image courtesy Tony Aymat
1. Swelling (oedema) at the back of the
larynx
2. Reddening (erythema) around structures
at the back of the larynx
A feeling of a lump in the throat is a very common symptom which can be linked to LPR and GOR. It is often called globus pharyngeus. Other people describe a feeling of tightness or constriction in the throat, or report a feeling of mucus sticking that they are unable to clear. Many people become concerned that they may have throat cancer although, in fact, the "lump in the throat" feeling is rarely a symptom in cancer cases. Stress can make this sensation worse: this is illustrated by the many English sayings that describe it so well. For example "I was so upset it brought a lump to my throat" "That really sticks in my throat" "I felt all choked up" "I can't swallow that". The important thing to realize is that globus is just an abnormal sensation of a lump rather than an actual lump or growth.
How is LPR diagnosed?
LPR is usually diagnosed by examination of your throat and voice box by an Ear, Nose and Throat (ENT) doctor using a small camera on a thin flexible fibre optic telescope passed through the nose. The ENT doctor or the Speech and Language Therapist (SLT) specialising in voice disorders will ask you to describe your symptoms. They may also ask you to fill in a questionnaire to rate how often and how badly your symptoms affect you.
What tests might my doctor order?
If your symptoms are severe, your doctor may send you for further tests to measure the acid level in your throat and gullet, and if, necessary, refer you to a gastroenterologist (a doctor specialising in stomach and digestive problems).
What causes LPR?
Often it is not clear what causes LPR. There may be a number of underlying causes, such as problems with the stomach, the gullet or the sphincter muscle (known as the cardiac or lower-oesophageal sphincter (LOS)) that separates the two. But, in many cases, lifestyle factors such as being overweight, smoking and consuming too much alcohol and caffeine are probable causes. Dietary factors may also play an important role and spicy or fatty foods, chocolate and citrus juice are frequently reported as contributing to symptoms of LPR.
How is LPR treated?
Treatment is usually planned on an individual basis and your doctor or SLT will suggest the appropriate treatment for you. There are several treatments that are effective:
- Making lifestyle and dietary changes
- Taking medications to reduce stomach acid or to discourage the stomach contents from spilling back
- Surgery is occasionally recommended to tighten the valve between the stomach and the gullet if medication has not been effective.
Most people with LPR need to modify how and when they eat, as well as taking some medication to help them.
Sometimes, non-prescription antacids/alginate preparations (e.g. Gaviscon Advance) are recommended. These work by forming a 'raft' over the stomach contents so that if anything spills back it is less damaging. This treatment is often very effective as the enzymes and bile contained in the stomach juices may cause more damage for many people than the acid. These should be taken four times each day – 10ml after each meal and 20ml at bedtime. Simple antacids without alginate (e.g. Maalox or Rennies) are much less effective and therefore not recommended to treat LPR. If you are already taking medication for other conditions, please consult your doctor before trying over-the-counter reflux medications.
For other patients, tablets that reduce the acidity of stomach juices will be recommended. These are known as proton pump inhibitors – PPIs – (e.g. omeprazole, lanzoprazole, esomeprazole). One dose in the morning and one in the evening (30 min – an hour before food) is usually recommended to treat LPR but regimes may vary for different individuals. These medicines can only be prescribed by your doctor and you should always take them as recommended. Sometimes a combination of PPI's and antacid/alginate preparations is recommended. Your doctor will help you find the right combination of treatment that suits you.
Most people with LPR report improvement in symptoms after 2-3 months of treatment but it may take 6 months or longer for the throat and voice symptoms to improve. Stopping reflux medications suddenly can increase LPR – a condition sometimes called rebound hyperacidity – and so most doctors recommend a 'step-down' plan. This ensures that the reflux control is maintained and that your symptoms do not re-occur. Your doctor will give you clear advice about how to stop taking your prescribed medication and you should make sure you follow it.
What can I do to reduce LPR?
There are things you can do to reduce the likelihood of reflux and also to reduce the amount of acid produced in the stomach:
- Give up smoking – smoking makes you more likely to reflux. You will probably have some LPR after every cigarette. Ask about your local smoking cessation clinic.
- Eat a healthy diet and adapt your eating habits.
- Limit your intake of fatty, fried and spicy foods, chocolate, cheese and pastry as these are all associated with increased reflux.
- Coffee, citrus juices and any form of fizzy drink can make reflux worse as they have been found to increase the level of stomach acid. Drink water or herbal teas instead.
- Chewing gum containing bicarbonate of soda (sold as tooth whitening gum) can be helpful.
- Eating smaller meals more regularly will help, as will eating slowly, chewing each mouthful well. Large meals cause more stomach acid to be produced and put additional strain on the valve between the stomach and the gullet.
- Leave 3 hours between eating and lying down.
- If you are overweight, try to lose weight (but note that extreme physical exercise can also cause reflux).
- Drink less alcohol, especially before bedtime, since alcohol makes reflux worse. Spirits and white wine are the worst offenders.
- Raise the head of your bed about 4-6 inches (place blocks under the legs/base of the bed at the head end). By raising your whole chest, gravity reduces the chance of acid travelling up to the throat while you sleep.
- Bend at the knees when you pick things up. If you bend at the waist, this puts pressure on your stomach contents, and leaning over forces acid up the gullet towards the throat.
- Wear loose clothing around your waist. Tight clothes put pressure on the stomach contents and can push acid up the gullet.
Will I always need treatment for LPR?
Usually LPR improves with the appropriate treatment but you need to:
- Follow the recommendations you are given on lifestyle changes.
- Make the dietary changes that are recommended.
- Take your medication regularly as prescribed by your doctor.
- Request review by a specialist centre if your symptoms do not improve with treatment.
- Remember that any decision to stop treatment should be made with your doctor's knowledge and consent.
In one way, having LPR and reflux is a little like having high blood pressure – with treatment it does not usually cause serious medical problems, but without treatment LPR can be serious, even dangerous.
For people with severe LPR or people who cannot take reflux medicine anti reflux surgery (to restore a new and better stomach valve) may be recommended. In people who have this surgery, most get good relief from LPR for many years.
This information is intended for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.

 Join us Now!
Join us Now! our newsletter
our newsletter free voice care leaflets & information – download here
free voice care leaflets & information – download here Help our work by donating while you shop
Help our work by donating while you shop