Voice care
See also free voice care literature and UK Voice Clinics directory
Paralysed Vocal Folds and Voice
by Sara Harris, Speech and Language Therapist specialised in Voice Disorders and Sara Caldwell, Speech and Language Therapist specialised in Voice Disorders. With grateful thanks to Cathinka Guldberg, Speech and Language Therapist specialised in Swallowing Disorders, Tom Harris, ENT Surgeon/Laryngologist and John Rubin, ENT Surgeon / Laryngologist.
What is a paralysed vocal fold (cord)?
A paralysed vocal fold (or cord), also often referred to as a vocal fold palsy, occurs when the nerve to one (or both) of the vocal folds cannot function. Nerves conduct electrical 'messages' or impulses from the brain to muscles so that they contract to make movements. If a nerve does not function, the muscles are not activated and lose their ability to move. If one vocal fold cannot move into the midline to meet the opposite fold, the voice will become weak, breathy and unstable in pitch. The nerves that supply the vocal folds are called the Recurrent Laryngeal nerves.
Why do vocal folds sometimes become paralysed?
Paralysed vocal folds are relatively rare. The most common cause is a simple viral infection. Viruses can sometimes 'attack' nerves during upper respiratory infections affecting their ability to function. This can sometimes happen to other nerves as well causing symptoms such as loss of smell or a facial paralysis known as Bell's palsy. Where the damage to the nerve is only partial, the affected vocal fold can still move, but its movement is slower and weaker in comparison to the normal fold and the effect on the voice is less severe. However, it will still be noticeable especially during periods of heavy or sustained voice use or in singing.
The recurrent laryngeal nerves that control the movements of the vocal folds are branches from a larger nerve called the Vagus nerve. The pathway of the left and right recurrent laryngeal nerves is different.
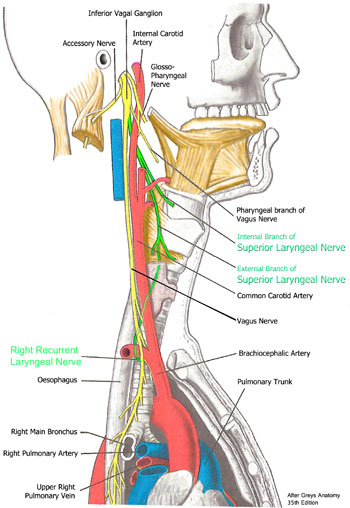
The right recurrent laryngeal nerve (shown in green) leaves the Vagus at the base of the neck and passes upwards into the larynx.
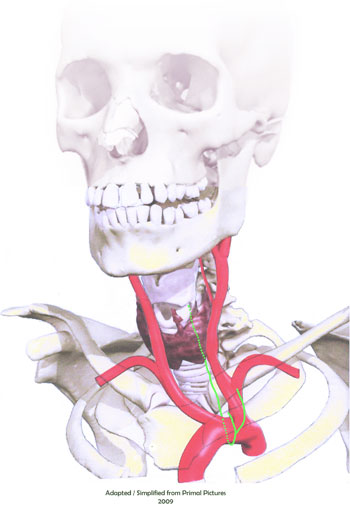
The left recurrent laryngeal nerve (shown in green) travels down into the chest cavity before leaving the Vagus, looping over the aorta (the main blood vessel leaving the heart) and travelling back up to the larynx.
They can sustain damage anywhere along their pathway to the larynx as a result of either direct injury or from compression sustained as a result of swelling or the growth of a cyst/tumour. There are other branches from the Vagus nerves that serve the swallowing muscles in the pharynx and the crico-thyroid muscles (the Superior Laryngeal nerves) that control pitch change for voicing. If the Superior Laryngeal nerves are damaged, the vocal folds are not paralysed but the voice will be affected as it will make the upper pitch range difficult to access. This will be of particular interest to singers and actors as it will affect their ability to perform.
Surgery to the neck, particularly surgery to the thyroid gland, sometimes results in a vocal fold paralysis. The thyroid gland lies very close to the lowest laryngeal cartilage (the cricoid cartilage), and the recurrent laryngeal nerve runs directly behind it. The nerve is therefore more vulnerable to bruising and compression during thyroid surgery that may cause it to temporarily malfunction. Normally, as the bruising and swelling subsides the nerve recovers its function and the vocal fold movement returns to normal. Direct trauma to the nerve is also a common cause of vocal fold paralysis. Blows to the larynx during contact sports such as rugby or judo, or compression from a seat belt during a car accident would be examples.
Because of its longer pathway, the left recurrent laryngeal nerve is exposed to greater risk of damage than the right. For example, surgery to the chest, heart, aorta or lung, or compression anywhere along its pathway may affect its ability to function. This is why your ENT surgeon will investigate your neck and chest with X-rays or CT/MRI scans to make sure nothing is affecting the nerve along it's pathway to the larynx.
The laryngeal nerves may also be affected as a part of a more general neurological disorder such as Multiple Sclerosis, Motor Neurone Disease or Parkinson's disease.
How will the paralysed vocal fold affect my voice?
The effect on voice quality may vary considerably from person to person, depending on where the affected vocal fold comes to rest in the airway. If it paralyses at or near its closed position in the midline, it will still usually be able to make good contact with the working fold and the voice may sound normal. However, the voice is still likely to fatigue more easily when used for long periods and particularly when used loudly to compete against noise.

Right vocal fold paralysis in breathing – paralysed fold close to the midline.

Vocal fold paralysis in voicing with potential for good closure.
If the paralysed fold comes to rest nearer its open position for breathing the voice is likely to be more severely affected. In this situation, although the working fold can still move normally to the midline, it cannot make contact with its paralysed partner. As a result, air from the lungs will escape through the wide gap between the vocal folds and the voice will sound extremely weak and breathy. Because a paralysed vocal fold often loses its usual muscle tone, it may become thinner and more bowed than its normal partner and the two folds will tend to vibrate at different pitches so that two differently pitched notes can be identified in the voice. This is known as diplophonia.

Left vocal fold paralysis close to the open (breathing) position. Note the thin bowed appearance of the paralysed fold.

Left vocal fold paralysis in voicing with poor closure. Note the recruitment of surrounding muscles.
When the paralysed vocal fold comes to rest somewhere between these two extreme positions the effect on the voice will depend how closely the vocal folds can approximate to one another. The closer they are to one another the better the voice is likely to sound.

Paralysed right vocal fold: paralysed fold lies between the open and closed position in breathing.

Well compensated right vocal fold paralysis in voicing with good closure. Note the minimal posterior gap and the compensatory movement of the left fold across the midline.
When the vocal folds cannot make contact with one another other muscles in the larynx may be recruited to try and help improve the closure. The false folds (or ventricular bands), which lie above the true folds, begin to move towards the midline and often appear enlarged. They tend to obscure the view of the true folds and at times may even come into contact with one another producing a low, rough, gravelly quality to the voicing. Whenever muscle recruitment occurs the voice quality deteriorates and voicing is usually described as feeling effortful, tiring and uncomfortable to produce.
Does a paralysed vocal fold affect me in any other way?
Some people notice that swallowing is more difficult. Food and particularly liquids may 'go the wrong way' causing coughing or choking. The throat may not feel completely clear after eating or drinking so that a second swallow is necessary to clear the throat. If swallowing is a problem a Speech and Language Therapist specialised in swallowing disorders can assess the problem and provide advice, exercises and strategies to help you compensate while the weakness recovers.
Lifting heavy loads may seem more difficult. This is because we rely on closing the vocal folds firmly together to build up pressure in the chest to give us extra strength to move heavy loads. If the vocal folds cannot close the pressure is lost and strength is reduced. Some people may notice they are more breathless with exercise or even when walking up stairs. If one vocal fold is paralysed close to the midline and cannot retract to its open position the airway is effectively reduced by half, making fast breathing more effortful.
How long does it take for the voice and swallow to recover?
In many cases the damage to the nerve is only temporary and the voice and swallow recover quite quickly over several days or a few weeks. The majority of people who suffered viral damage or bruising to the nerve during surgery will have largely recovered somewhere between three to nine months post onset. However, for some people the recovery may be slower and continue for up to 12-18 months. Where the nerve has been severely damaged or severed it cannot recover and the paralysis is permanent. If there has been little or no improvement in the paralysis after a year from the onset that paralysis is also considered to be likely to be permanent.
What can be done to help a paralysed vocal fold and improve the voice?
Voice therapy from a voice specialised Speech and Language Therapist can improve the voice quality and reduce the effort of speaking in most cases. It is important to try this option first, particularly if the vocal folds are near to the midline. Vocal exercises help:
- The working fold compensate by moving across the midline to make contact with the paralysed fold
- Improve swallowing difficulties.
- Reduce excess tension and the recruitment of other laryngeal muscles
- Improve the voice quality and reduce feelings of strain and discomfort.
If you are a singer it may be more difficult to control vocal intensity and the stability of pitch. It may also be more difficult to raise the larynx and use the pharyngeal muscles in the throat to 'tune' resonance for vocal brightness. You may also find your voice fatigues quickly and sounds weaker and breathier than usual. It is especially important for singers/actors/performers to work on their voices with a Speech therapist and a singing teacher/voice teacher experienced with voice rehabilitation.
In cases where there is significant excess muscle tension interfering with vocal function laryngeal manipulation and massage from a voice specialised osteopath or physiotherapist can be helpful.
If the paralysed vocal fold fails to recover and voice therapy has failed to help the working fold compensate, surgery may be recommended. There are many good surgical techniques that can be used to bring the paralysed vocal fold towards the midline to approximate with the working fold. You will need to discuss which type of surgery is likely to suit your situation best with your ENT Surgeon. Surgery may not result in a normal voice but it usually improves vocal quality and intensity (loudness), increases vocal stamina and decreases strain and discomfort.
What can I do to help myself?
- Try not to whisper. Speak as normally as you can rather than force your voice to be louder. Attempts to speak loudly usually make the voice sound worse.
- Make sure you have your listener's attention and face them while you speak.
- Avoid noisy surroundings where possible
- Make sure your friends know that your vocal fold is paralysed and that you cannot speak loudly so they make allowances and don't speak over you.
- If you are a singer continue to work on vocal exercises and try to keep singing to help maintain the muscle tone. Be prepared to accept your voice will not be at its best.
- If you need to lift things reduce the load into smaller less and make more journeys
- If your paralysed vocal fold makes you more breathless pace yourself by going a bit slower on stairs or up hills and give yourself time to adapt your breathing
- If you have problems with swallowing make sure you sit upright while eating and don't try to eat and talk! Ask for a referral to a Swallowing specialist Speech Therapist.
- Make sure you eat and drink more slowly taking smaller, more manageable mouthfuls.
- Try to avoid foods with a mixture of solids and liquids, (eg cereal with milk, or meat with thin gravy). While you are chewing solids the liquid and may 'go the wrong way' and cause coughing/choking.
Note re. images: Images of the vocal folds taken during a laryngeal examination appear to be inverted (upside down) from the patient’s perspective. The right vocal fold therefore appears on the left side of the picture and vice versa.
This information is intended for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.

 Join us Now!
Join us Now! our newsletter
our newsletter free voice care leaflets & information – download here
free voice care leaflets & information – download here Help our work by donating while you shop
Help our work by donating while you shop